Crohn’s disease is a chronic condition that affects the digestive system. It can cause ulcers, inflammation, and various other symptoms. According to experts, Crohn’s disease is an inflammatory disease that can be debilitating and painful and sometimes lead to life-threatening complications.
As an autoimmune condition, it can be unpredictable, leaving you feeling normal one day and in pain the next.
Around 1.4 million Americans live with the condition, but despite its prevalence, there are many things about Crohn’s disease that people don’t know. In this article, we will discuss 10 of them. Keep reading to find out more information on this debilitating condition!

1. It’s different for everyone
Crohn’s, an autoimmune condition, is a type of inflammatory bowel disease (IBD). In people who have it, the immune system attacks the gastrointestinal (GI) tract now and again, leading to inflammation. These bouts, or flares, cause symptoms including abdominal pain, diarrhea, rectal bleeding, and fever.
Crohn’s can occur anywhere in the digestive system, but in about 70% of cases, it affects the top of the large intestine and the bottom of the small intestine. This is called ileocolonic Crohn’s. Around 30% of patients have Crohn’s colitis, which affects only the large intestine.
The symptoms can be different depending on the location of the disease within the body, the response to treatment, and the severity of the symptoms. But these factors can differ significantly even among people with the same type of Crohn’s disease. Experts don’t know exactly what causes these differences.
2. You probably don’t have to restrict your diet
As long as you’re not having a bout of Crohn’s, you probably don’t need to restrict your diet. According to doctors, there are many diets out there that focus on reducing Crohn’s disease’s symptoms. However, they point out that since different patients experience the condition so differently, a diet that may work for one individual may not work for somebody else.
If your Crohn’s is active, of course, you should avoid foods that may make it worse. These include caffeine, milk, and certain high-fiber options such as popcorn and nuts. As long as it’s inactive, though, it’s fine to eat a wide range of healthy foods.
In fact, dietitians say that complex, rich foods—such as whole grains, nuts, and dairy products—can help exercise your GI tract. They also mention that you wouldn’t tell someone with cardiovascular disease to completely stop exercising so as not to stress their heart. Similarly, people with Crohn’s disease need some exercise in the GI tract.
3. It’s not your fault you have Crohn’s
Even though certain foods can worsen flare-ups, experts say that diet isn’t the root cause of Crohn’s disease.
Many patients think that their condition is their fault, but we’re here to tell you that it isn’t anything you did wrong or anything you ate. It’s your genes combined with certain environmental factors that trigger an autoimmune response.
By the way, this recipe book has plenty of recipes for those living with Crohn’s disease; you should give it a try!
4. Treatment should be tailored to your life
There are many different biologics available, including certolizumab (Comzia), adalimumab (Humira), and infliximab (Remicade). Another is ustekinumab (Stelara), which was approved by the FDA in September 2016 for the treatment of Crohn’s disease.
Experts say that, when deciding which treatment may be best for which patient, it’s important to consider more than just the condition. Adalimumab and infliximab, for example, are also used to treat rheumatoid arthritis, psoriasis, and ankylosing spondylitis. Ustekinumab is also used to treat plaque psoriasis.
For Crohn’s patients who have skin lesions or joint pain, a medication that also targets those health issues can be a great decision.
Also, the way the medication is administered differs depending on the treatment. You take infliximab only once every eight weeks, but you need to visit an infusion center to do that. Adalimumab is an injection you give yourself, but you have to take it once every week or two.
For instance, for someone who travels a lot and has Crohn’s disease, making it to an infusion center every eight weeks can be difficult. That’s why injectable medication is a better choice.

5. Medication can—and should—be tailored to your type of Crohn’s
While experts haven’t found yet a cure for Crohn’s, medications can prevent flares most of the time. However, like the condition itself, the right treatment varies from patient to patient.
For those with Crohn’s colitis, doctors usually start with a type of medication called 5-aminosalicylate acid (5-ASA), which reduces the inflammation of the intestinal lining.
While this medication is good at soothing inflammation of the colon, it doesn’t work well on the small intestim. For patients whose condition affects any part of their small intestine, doctors typically start with a biologic, which helps prevent inflammation, an immunomodulator, which suppresses the immune system, or a combination of the two.
6. If medications don’t work, there are other options
If medications seem to not have the expected effect, your doctor may recommend surgery. While this may sound scary at first, it isn’t. This type of intervention is easy, with little to no risk.
Around two-thirds of people with Crohn’s disease need surgery at some point, generally to remove damaged parts of the intestine.
7. Remission doesn’t mean you should stop taking medication
Crohn’s disease often goes into remission with the right treatment. However, this doesn’t mean that you can stop taking it.
Doctors warn that stopping medication, even in patients who are inactive, has been linked with a 40–50% risk that they are going to have a bout of Crohn’s the following year. And a flare of it can lead to hospitalization, surgery, and other complications.
Nevertheless, a small number of people are able to stop taking medication, especially those who haven’t had flares for several years.
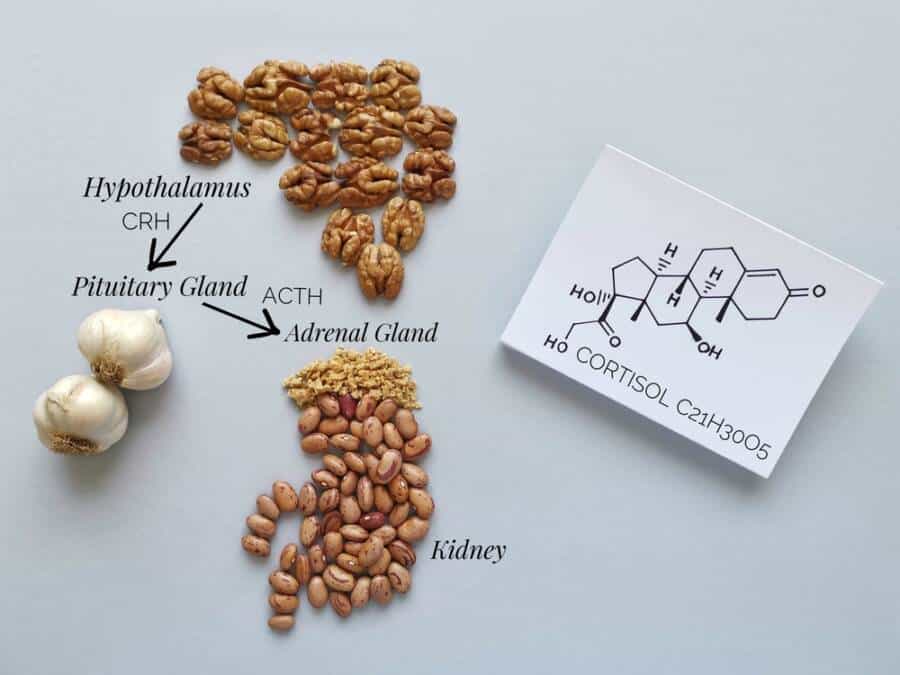
8. Reducing stress can decrease the risk of having a flare
Scientists have found that stress-reducing activities can improve the quality of life for people with Crohn’s disease and lower the risk of having a flare. These activities may include exercising, listening to music, doing yoga, meditating, or doing another relaxing activity you enjoy.
Experts also recommend attending a support group. Even though the condition is different for everyone, it’s often a huge relief to have the chance to talk with others and share experiences and stories. Basically, it shows you that you’re not alone in this.

9. Good sleep habits can also help prevent flares
Along with stress, poor sleep habits can cause Crohn’s disease. Even when the condition is inactive, many patients experience fatigue and sleep disturbances. To soothe these issues and help prevent future flares, experts advise people to develop “extremely regimented” sleep habits.
This usually means going to sleep and waking up at the same time every day—yes, including weekends. Another thing that may help is making sure you’re sleeping seven to nine hours each night. According to several studies, patients with irregular sleep schedules and people who don’t get enough sleep have more active diseases.
If you have trouble falling asleep, pay attention to your light exposure, which is the main driver of your body’s internal biological clock. This being said, limit nighttime light exposure and avoid screens before you go to bed. In the morning, make sure you get enough light to start your circadian clock. Open your windows and let the morning light come in.
10. You don’t need to stop drinking
According to some experts, drinking is okay for those with Crohn’s disease. In clinical studies, they found that moderate alcohol intake (two drinks a day for men or one for women) doesn’t harm patients with the condition. Moreover, it turned out that drinking alcohol may even have benefits since it slightly suppresses the immune system.
However, this is true only if you don’t consume too much. Heavy drinking is often associated with increased intestinal permeability, which occurs when the intestines allow substances to pass through them and travel to other parts of the body. This can eventually lead to flares.
If you liked our article on Crohn’s disease, you may also want to read 8 Best Arthritis-Friendly Foods for Joint Relief.